On January 8, 2024, CorrectSequence Therapeutics Co., Ltd. (Correctseq), a ShanghaiTech spinoff, using innovative transformer Base Editing (tBE) technology to help people with severe diseases, announced positive results of its base editing therapy for transfusion-dependent β-thalassemia, CS-101. As a collaboration with the First Affiliated Hospital of Guangxi Medical University, the Investigator-Initiated Trial (IIT) of CS-101 has successfully cured the first treated patient with transfusion-dependent β-thalassemia, resulting in sustained transfusion-free for more than two months. Eight weeks after CS-101 treatment, the patient’s fetal hemoglobin (HbF) level has increased to ~95 g/L, accounting for ~81% of total hemoglobin. The percentage of HbF-expressing cells (F-cells) has increased to ~80%. Up to the reporting date, the patient’s hemoglobin level has been maintained at or above 130 g/L, and the patient has resumed normal life. Notably, to the best of our knowledge, this is the world’s first report of successful clinical cure of hemoglobinopathy with base editing therapy.
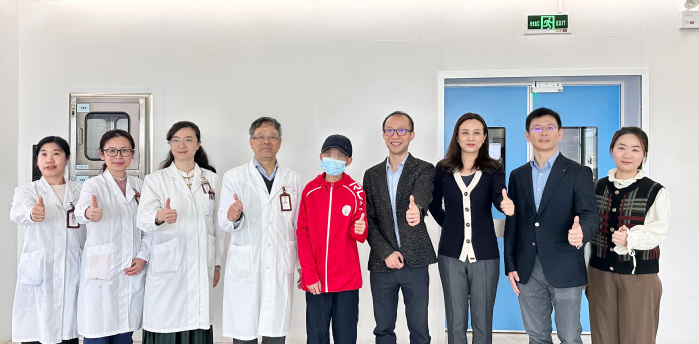
The world’s first β-thalassemia patient who received base editing therapy (Correctseq’s CS-101) has been two months free from transfusion and has resumed normal life.
Encompassing β-thalassemia and sickle cell diseases (SCD), hemoglobinopathies are the most common group of monogenic diseases in the world, with about 7% of the global population carrying the mutant gene. About 400,000 newborns are with hemoglobinopathies every year worldwide. β-thalassemia is a genetic disease caused by mutations in the β-globin gene, resulting in defective hemoglobin production. Correctseq’s CS-101 is a personalized treatment that begins with the collection of autologous hematopoietic stem cells from β-thalassemia patients. The transformer Base Editor (tBE) technology (Wang et al., Nat Cell Biol, 2021), developed by scientists at ShanghaiTech University, is then used to precisely edit the DNA sequence of the promoter region of the gene encoding γ-globin (HBG1/2) to mimic the naturally occurring single-nucleotide variant in the population with hereditary persistence of fetal hemoglobin, thereby reactivating the γ-globin expression to produce functional HbF. Finally, the edited stem cells are infused back into the patient, enabling the patient to continuously produce blood cells with intact hemoglobin and eliminating the need for frequent blood transfusions. While several gene editing strategies have been explored to restore normal hemoglobin levels in β-thalassemia patients, it has been shown that base editing of the BCL11A binding site at the HBG1/2 promoter by tBE—as in the CS-101 treatment—exhibited the highest level of γ-globin reactivation both in vitro and in vivo (Han et al., Cell Stem Cell, 2023).
In Correctseq’s CS-101 IIT study, the first patient who suffered from transfusion-dependent β-thalassemia (β0/β+ type) received the tBE-based gene editing therapy in October 2023. This patient began receiving blood transfusions at the age of two and had been receiving 4 units of red blood cells (RBC) every two weeks before beginning CS-101 treatment. After receiving CS-101 treatment, the patient successfully achieved hematopoietic reconstruction, with neutrophil engraftment occurring within 16 days, and stopped receiving blood transfusions at day 14 post-transplantation. Four weeks after treatment, the patient’s HbF concentration was ~16 g/L, representing ~21% of total hemoglobin, and the F-cell ratio was ~23%. Eight weeks after treatment, the patient’s HbF concentration increased to ~95 g/L, representing ~81% of total hemoglobin, and the F-cell ratio was ~80%. Up to the reporting date, the patient’s hemoglobin level has been maintained at or above 130 g/L, and no adverse effects related to CS-101 have been observed.
Compared with other CRISPR-based β-thalassemia gene editing therapies, CS-101 using tBE technology shows effective hematopoietic reconstruction, earlier recovery to the normal range of hemoglobin level, and shorter time to achieve transfusion independence. Importantly, CS-101 does not harbor safety risks such as large DNA fragment deletions, chromosomal rearrangements, or off-target mutations, owing to the innovative tBE technology. As a result, Correctseq’s CS-101 has the potential to become the best-in-class gene editing therapy and first-in-class base editing therapy for β-hemoglobinopathies.
The success of Correctseq’s CS-101 IIT study offers great hope towards a cure for patients with β-hemoglobinopathies. In addition to this first adolescent patient who was successfully cured, one adult patient has been free from transfusion for more than one month after receiving CS-101 treatment. The ongoing IIT study is expected to yield further promising results. CS-101 is now entering IND stage, which will enable treatment of additional patients and further assessment of safety and efficacy. An investigational study using CS-101 to treat patients with SCD is also under active preparation. Correctseq is determined to efficiently promote the clinical translation of innovative gene editing technologies, bringing hope for “one-time treatment, life-time cure” to patients with severe diseases worldwide.
*This article is provided by CorrectSequence Therapeutics